The growing use of smart technologies built with artificial intelligence (AI) is revolutionizing the world and how people live in it. AI is making people’s lives easier and more convenient. Beyond consumer living, advanced technologies based on AI, machine learning, big data analytics, and the Internet of things have paved the way for the development of sophisticated applications designed for specific environments such as manufacturing, logistics, and planning, as well as business operations. They are used to improve manufacturing processes, provide more sophisticated data analytics, automate manual tasks and improve quality control. Known as the Fourth Industrial Revolution (4IR) era, these technologies and devices are widely applied for innovation and value creation across many industries.[1]
The use of AI applications in the healthcare industry is also rapidly expanding. Widespread applications of advanced technologies and AI in healthcare institutions are supporting efforts to improve care, service quality, and the efficiency of medical resources and staff. The adoption of some of these technologies in radiology has not only been effective in optimizing workflows with patient positioning and protocol assistance but also dose tracking and reporting.
In the past few decades, developments in medical imaging technology and the increased role of imaging within the diagnostic process have resulted in a rapid expansion of recorded medical visual data, generating a need for novel computational models.[2] AI tools are helping radiologists process large volumes of imaging data with advanced image reconstruction algorithms and are helping to improve the consistency and accuracy of medical imaging and diagnostics. Several AI-based image analysis models, including machine learning, were developed to assist with image reconstruction. Unlike traditional, rule-based AI algorithms, the concept of machine learning lets the machines learn by themselves by ingesting vast amounts of data and detecting patterns. Many machine learning algorithms use statistics, formulas, and big data to function.[3]
The growing role of deep learning applications in medical imaging
Deep learning, a subset of machine learning, is considered by some to be an integral part of the 4IR.[4] It makes use of layers of information processing, each gradually learning more and more complex representations of data, and is a type of machine learning that uses complex neural networks to replicate human intelligence. A major breakthrough in the field of deep learning was the introduction of the convolutional neural network (CNN), now considered to represent the state of the art in image analysis.[5] Deep learning reconstruction is already being used in a number of imaging modalities, such as magnetic resonance imaging (MRI) and computed tomography (CT), and also holds potential in other imaging modalities, such as positron emission tomography (PET/CT).
GE Healthcare’s MRI deep-learning image reconstruction algorithm has evolved the MRI scanner’s capabilities to enable exceptional image quality without compromising scan time. In CT applications, GE Healthcare’s CT deep learning image reconstruction engine was trained using a library of thousands of low-noise, filtered back projection images considered the gold standard of image quality. Using this deep neural network results in high-quality images with reduced noise and artifacts. Advances like these have enabled compelling results thus far, and powerful improvements can be seen in image quality and resolution that were made possible using deep-learning image reconstruction techniques. Industry leaders are continuously striving to develop deep-learning solutions that can be applied in healthcare, specifically radiology.[6] Deep learning is an important application of AI and now, a new frontier of machine learning is being explored in PET/CT to enhance image processing capabilities across molecular imaging systems.
“The evolution of AI technologies in medical imaging has dramatically influenced the way clinicians can visualize disease,” said Erez Levy, General Manager for Molecular Imaging at GE Healthcare. “We are continuing to innovate in PET/CT with the addition of exciting new digital and AI technologies such as deep learning image processing. We’re committed to delivering on the promise of expanding PET/CT’s diagnostic capabilities and preparing the technology for a sustainable future, where its application in emerging areas such as theranostics is still evolving.”
As PET/CT technology evolves with advanced imaging detector hardware, more imaging data is generated that can be used in image reconstruction techniques. A quantum leap in AI innovation, new deep-learning solutions available via imaging software can replicate the image quality performance benefits produced by the most sophisticated PET/CT detector technology, making the high-quality imaging and clinical information generated by these systems more accessible for more patients.
Advancing PET detector capabilities for improved accuracy
Since their introduction into routine clinical use, hybrid molecular imaging technologies such as PET/CT have advanced complex diagnostics and disease staging by enabling improvements in specificity and quantitation. Over time, advances in PET/CT hardware and software led to significant enhancements in image quality and clinical workflow improvements. Digital detectors replaced analog photon-counting techniques to enable further improvements in specificity and quantitation, which also enabled shorter scan times, improved small-lesion detectability, and reduced radiation dose for the PET portion of the exam, enabling improved image quality.[7]
As with all modalities of imaging equipment, PET/CT technology is quickly moving in the direction of improved diagnostic accuracy. For PET/CT imaging, one of the biggest steps in that direction has been the development and proliferation of Time-of-Flight (TOF) technology.
PET detectors capture and measure the two annihilation photons, or counts, that are produced back-to-back after positron emission from the tracer molecule, which is chosen to highlight a specific function in the body on a biochemistry level. The photons released are detected by coincidence imaging as they strike scintillation crystals.[8]
The added benefit of TOF PET/CT imaging is that it illustrates timing resolution and infers when and where each annihilation event occurred on the line of response between the two detectors. It can improve the accuracy of a lesion uptake measurement through better signal localization and reduced noise propagation.[9]
Evolving PET/CT with deep learning innovation
Innovating PET/CT with TOF capabilities has certainly enhanced clinical diagnostics since it was introduced, but innovations in PET/CT imaging technology continue. Industry leaders such as GE Healthcare have introduced a game-changing new PET/CT imaging platform that brings together the highest PET sensitivity* levels with TOF image quality performance benefits via deep-learning image processing.
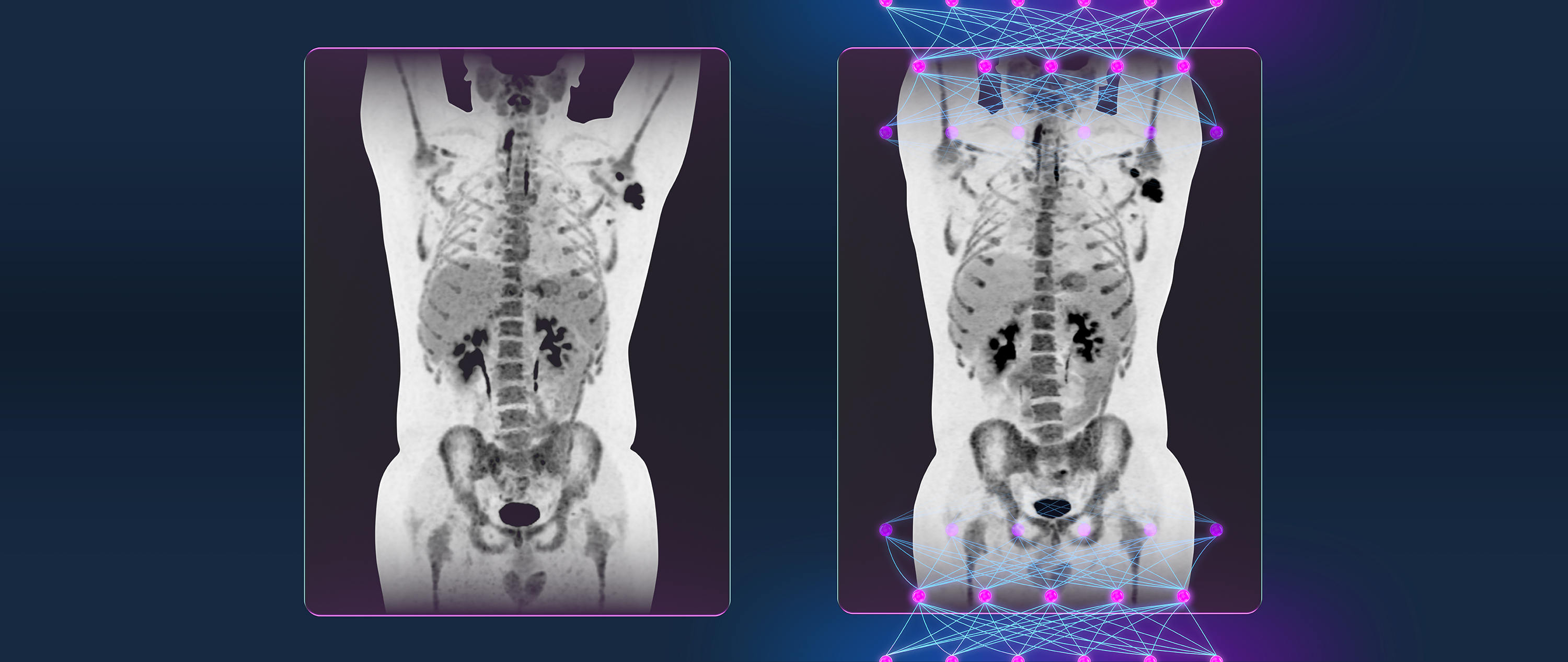
The new PET/CT platform was built to exceed industry sensitivity standards, creating the potential to image high count rate tracers beyond 18F-fluorodeoxyglucose (FDG) as they are developed and utilized in clinical PET/CT imaging. TOF image quality performance benefits in the new system are made possible with an innovative deep-learning solution designed to increased small, low-contrast lesion detectability compared to Time-of-Flight systems.**
Unique in molecular imaging, the system’s deep learning image processing is achieved using a CNN, trained on thousands of PET/CT images constructed via various reconstruction methods, including TOF. The CNN learns the characteristics of each image; therefore, the resulting images provide image quality performance benefits most associated with hardware-based TOF systems, such as better contrast-to-noise ratio and contrast recovery.w Deep learning techniques using CNNs enhance images with the image quality performance benefits most associated with TOF without investing in more hardware or new equipment.
Enabling precision medicine with innovations in PET/CT
Continuous innovation in molecular imaging technology is paving the way to a future where the standard of care is selecting the most effective treatment for each individual patient. From cancers to chronic diseases, clinicians are utilizing molecular imaging to support precision diagnoses and to develop targeted therapies for individual patients that may help lead to fewer side effects and better outcomes.
Forward-thinking molecular imaging innovations such as deep-learning-based image processing has the potential to enable broader access to advanced imaging technologies and novel AI techniques that can learn and replicate the enhanced image quality performance benefits typically generated by specific hardware.
The diagnostic power of PET/CT imaging will continue to play a key role in enabling precision medicine and benefits from the evolution of improvements in the system’s hardware and software capabilities to continually enhance image quality and to improve access to this powerful technology. Enhancing system capabilities with sophisticated AI-based technologies such as deep-learning moves molecular imaging into a future where it can further impact precision diagnostics and precision medicine.
Learn more about GE Healthcare’s latest PET/CT, Omni Legend to help advance your patient outcome.
DISCLAIMERS
Not all products or features are available in all geographies. Check with your local GE Healthcare representative for availability in your country.
Omni Legend and Precision DL are CE marked. Omni Legend is 510k-cleared by the US FDA. Precision DL is 510k-pending with the US FDA. Not available for sale in the United States. Clinical images shown was processed with Precision DL and obtained from an investigational device, limited by U.S. law to investigational use.
*Omni Legend 32 has highest sensitivity per cm for conventional (non-total body) PET-CT systems.
**At matched scan time and injected dose. Detectability using clinical data with an inserted 8 mm diameter liver lesion of known location and 2:1 contrast using a CHO model observer, comparing SNR from Omni Legend 32 cm with QCHD and Precision DL to SNR from Discovery™ MI 25 cm with QCFX.
wContrast recovery and contrast-to-noise demonstrated using clinical data with inserted lesions of known size, location, and contrast. Using data from Omni Legend 32 cm, CR and CNR were measured using H-PDL and QCHD
REFERENCES
[1] Lee D, Yoon SN. Application of Artificial Intelligence-Based Technologies in the Healthcare Industry: Opportunities and Challenges. Int J Environ Res Public Health. 2021;18(1):271. Published 2021 Jan 1. doi:10.3390/ijerph18010271
[2] Kruskal JB, Berkowitz S, Geis JR, Kim W, Nagy P, Dreyer K. Big data and machine learning-strategies for driving this bus: a summary of the 2016 Intersociety Summer Conference. J Am Coll Radiol 2017;14(6):811–817.
[3] https://www.techtarget.com/searchenterpriseai/tip/AI-vs-machine-learning-vs-deep-learning-Key-differences
[4] Hricak H. 2016 New Horizons Lecture: beyond imaging—radiology of tomorrow. Radiology 2018;286(3):764–775. Link, Google Scholar
[5] https://pubs.rsna.org/doi/full/10.1148/radiol.2018180547
[6] ibid
[7] Added Value of Digital over Analog PET/CT: More Significant as Image Field of View and Body Mass Index Increase
Shirin Hatami, Sarah Frye, Anna McMunn, Crystal Botkin, Razi Muzaffar, Kara Christopher, Medhat Osman
Journal of Nuclear Medicine Technology Dec 2020, 48 (4) 354-360; DOI: 10.2967/jnmt.120.244160. https://tech.snmjournals.org/content/48/4/354
[8] Jha AK, Mithun S, Puranik AD, Purandare NC, Shah S, Agrawal A, Rangarajan V. Performance characteristic evaluation of a bismuth germanate-based high-sensitivity 5-ring discovery image quality positron emission tomography/computed tomography system as per National Electrical Manufacturers Association NU 2-2012. World J Nucl Med. 2019 Dec 18;18(4):351-360.
[9] Karp JS, Surti S, Daube-Witherspoon ME, Muehllehner G. Benefit of time-of-flight in PET: experimental and clinical results. J Nucl Med. 2008 Mar;49(3):462-70. doi: 10.2967/jnumed.107.044834. Epub 2008 Feb 20. PMID: 18287269; PMCID: PMC2639717.