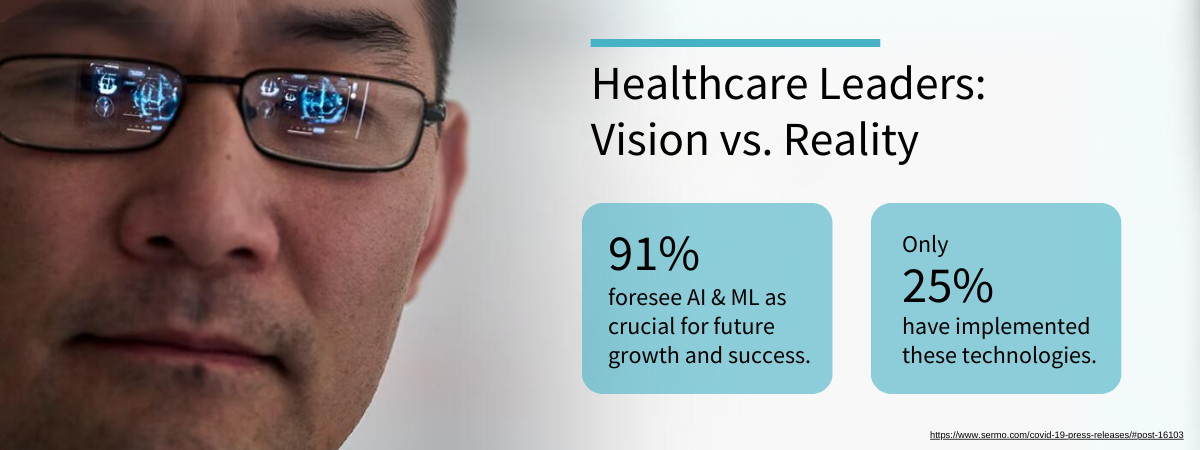
Artificial intelligence (AI) has become a ubiquitous term across industries, promising transformative capabilities in nearly every conceivable application. The healthcare sector, however, is navigating the early stages of this transformation. A recent Sermo survey of healthcare leaders at hospitals and other provider organizations unveiled a fascinating contrast: 91% of leaders surveyed believe AI and machine learning (ML) will be an integral part of their organization's growth and success in five years and beyond, but only 25% have implemented it.1
What’s the disconnect between aspiration and action? Healthcare leaders share in the challenge of determining the best entry point for AI integration. While potential benefits are clear—enhanced diagnostic accuracy, operational efficiency, and improved patient outcomes—AI initiatives must address key clinical and business challenges and seamlessly fit into existing workflows to drive adoption and deliver immediate value. Also, clinicians must trust that the AI they encounter is accurate.
Medical imaging and image acquisition is a prime candidate for AI adoption. Rising demands for diagnostics due to more specialized care, imaging in acute settings, and an increase in imaging-based screenings, coupled with cost and staffing constraints and technological advancements, are propelling this area of care toward a tipping point. Among the various imaging modalities, ultrasound workflows are particularly ready for AI-driven advancements and efficiencies.
Ultrasound utilization is expanding across hospital departments and care settings even though there is a shortage of well-trained and experienced ultrasound technologists. Demand for exams has led imaging departments to fast track novice techs into clinical roles. Point-of-care ultrasound (POCUS) devices have democratized imaging, offering real-time diagnostic capabilities in care settings such as emergency departments, intensive care units, orthopedics, cardiology, and internal medicine. It is a beneficial diagnostic tool to have during patient encounters, but the non-traditional operators capturing these images, such as physicians and nurses, may lack specialized training in acquiring diagnostic quality images and/or properly documenting ultrasound exams.
Ultrasound is a high-stakes art form
Ultrasound image acquisition is more than a technical procedure; it’s an art form that demands a blend of skill, experience, and intuition from the sonographer or clinician. Each scan is an exercise of movements and adjustments, where the operator’s knowledge and experience guide the transducer to capture the body’s story in waves and echoes. This intricate process relies heavily on the training of individuals who interpret the subtle interplay of anatomy and technology.
Capturing an incomplete or inadequate set of images during an ultrasound exam can have significant implications for the diagnosis and subsequent treatment. In medical imaging, each image serves as a crucial piece of the diagnostic puzzle, providing insights into the structure and function of internal organs, vasculature, bone, ligaments, and more. When anatomy is not adequately visualized there is a risk of missing important findings such as abnormalities, lesions, or pathologies. This can lead to a delayed or incorrect diagnosis, potentially resulting in ineffective treatment strategies or even compromising patient outcomes. An incomplete ultrasound exam can also necessitate additional examinations—commonly referred to as callbacks—which are inconvenient, unsettling, and costly for patients, and a redundant use of resources if unnecessary.
Incomplete ultrasound exams can also have financial implications. One study found that more than one in five radiology reports contain an error that can impact billing.2 If an ultrasound exam is deemed incomplete due to missing images or inadequate documentation, it may not be fully reimbursed. Physicians who fail to save images and clips into the ultrasound image archive are a major contributing factor in the approximately 77% of ultrasound exams in the ED that go unbilled.3 The need to manually perform measurements or interpret poor image quality can also impact the accuracy of radiology reports.4
AI-driven ultrasound tools
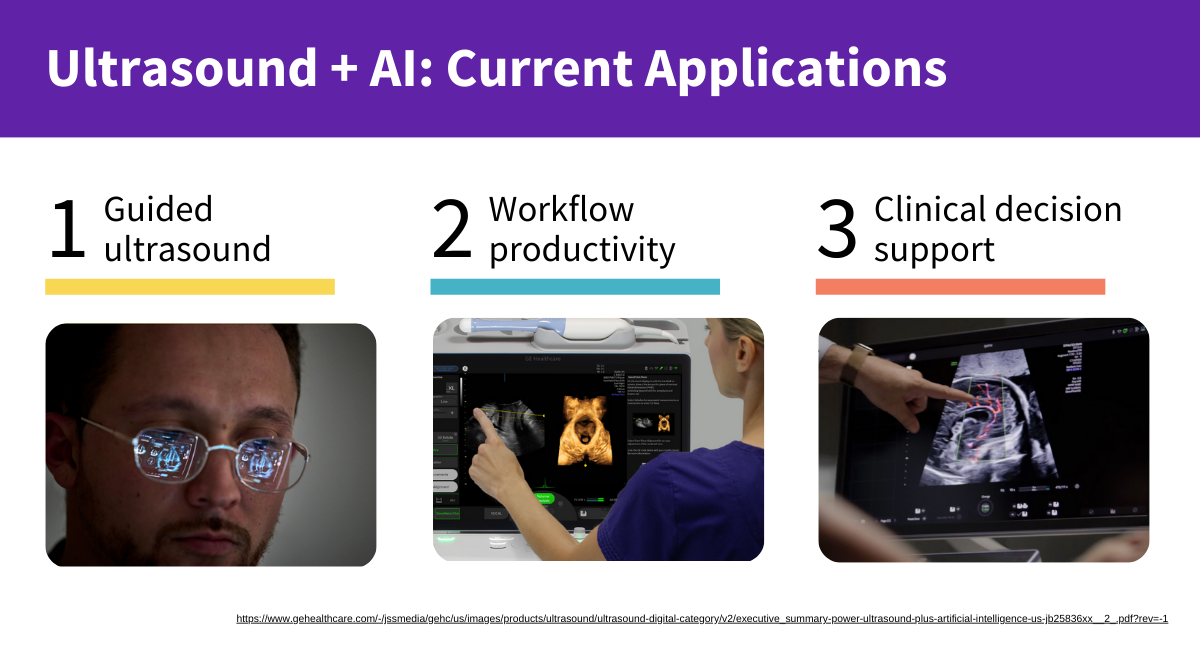
The combination of AI and ultrasound may seem futuristic, but it’s making an impact now. The current application of AI in ultrasound digital tools falls in three areas: guided ultrasound, workflow productivity, and clinical decision support.
Guided ultrasound
First, AI technology is available to provide real-time scan guidance to enhance operator efficiency, improve diagnostic accuracy, and enable more precise procedures. Device-based algorithms can analyze live ultrasound images to identify specific organs, blood vessels, or abnormalities and give the operator guidance and recommendations on probe positioning, imaging technique, and suggestions on additional views or measurements. Visual cues can highlight anatomical landmarks, target regions, or trajectory paths for procedures, and provide operators with an automated quality assessment.
One example of guided ultrasound, Caption Guidance, the first FDA cleared AI-guided imaging acquisition software, provides users with turn-by-turn on-screen guidance to capture diagnostic-quality cardiology scans. It provides prescriptive guidance, a quality meter, and can automatically select and save the best available image loop from the continuous recording for each view. It can support non-expert ultrasound users in the collection of echocardiography loops.5
Workflow productivity
Next, AI algorithms are boosting provider productivity by automating anatomical measurements. When performed manually, these tasks take time and can invite variability.
For example, AI enables more accurate and automated estimation of left ventricular ejection fraction in cariology6 and automatically detects and classifies endometrial thickness of ovarian cysts for OBGYN providers.7 Certain Versana ultrasound systems are enabled with AI to automate labeling of right upper quadrant organs, removing a number of manual steps in an abdominal exam. A Voluson™ AI capability removes the complexity of assessing pelvic floor anatomy and reduces exam time. AI can also have an impact on interpretation throughput; integrating AI into breast ultrasound screening has been shown to reduce radiologists’ reading time by 38% with no loss of diagnostic accuracy.8
Clinical decision support
Finally, AI algorithms can analyze ultrasound images and assist providers in identifying and interpreting abnormalities or subtle features that may otherwise be challenging to detect. In POCUS utilization, this may help physicians who have less experience interpreting ultrasound images diagnose diseases and conditions more accurately. Algorithms can highlight areas of concern such as tumors, cysts, or lesions, or provide real-time risk insight.
Tools such as Breast Assistant powered by Koios DS™ on GE HealthCare’s general imaging ultrasound LOGIQ™ platform and Invenia™ ABUS 2.0 help physicians confidently assess the malignancy of breast lesions, knowing that AI has compared their patient’s lesion to more than 400,000 other images. This diagnostic clarity can help physicians detect disease earlier and avoid unnecessary procedures and treatments on non-malignant lesions. One study using Breast Assistant powered by Koios DS found a cancer identification rate of nearly 100%, with a 69% reduction in benign biopsies.9 In near-real time, LOGIQ’s™ Thyroid Assistant, powered by Koios DS, automatically populates all TI-RADS® descriptors and generates an AI-based thyroid cancer risk assessment using machine learning and proprietary algorithms, leading to a 57% reduction in benign biopsies.10
AI-enabled digital ultrasound tools for consistent care
As healthcare provider organizations merge and integrate sites, the challenge of providing consistent care from sonographer to sonographer and across different locations becomes increasingly complex. Here, AI steps in as a vital tool in the effort to standardized care, helping to bridge the gap between disparate care locations and ensuring that the same excellent level of care is delivered no matter the clinician at the bedside or the site of service. As one example, an AI thyroid assistant was shown to reduce inter-reader variability by 41%.11 By implementing AI-driven protocols for ultrasound exams, organizations can ensure consistent image quality and reporting standards across all sites, effectively reducing the potential for variability and elevating the overall standard of care. This not only benefits patients by providing reliable and predictable outcomes but also streamlines the operational aspects of healthcare delivery, paving the way for a more efficient and unified healthcare system.
Learn more about the power of ultrasound + artificial intelligence.
REFERENCES:
1. https://www.sermo.com/covid-19-press-releases/#post-16103
2. Frequency and Spectrum of Errors in Final Radiology Reports Generated With Automatic Speech Recognition Technology; Quint, Leslie E. et al.; Journal of the American College of Radiology, Volume 5, Issue 12, 1196 – 1199.
3. Stephen Alerhand et. al., Attrition in emergency department point-of-care ultrasound workflow adherence for the evaluation of cutaneous abscesses, JHMHP 2020
4. Improving Accuracy in Radiology Images and Reports | GE HealthCare (United States)
5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7541096/
6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7541096/
7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7702141/
8. https://ajronline.org/doi/full/10.2214/AJR.18.19516
9. Love SM, Berg WA, Podilchuk C, Hovanessian-Larsen LJ, Dauphine C, Jairaj A, Barinov L, Hulbert W, Cen S, Eshraghi L, Mammone R. Automated, low-cost palpable breast lump triage for economically-developing countries [abstract]. In: Proceedings of the 2016 San Antonio Breast Cancer Symposium; 2016 Dec 6-10; San Antonio, TX. Philadelphia (PA): AACR; Cancer Res. 2017;77(4 Suppl): Abstract nr PD3-01
10. 2023; The AI-enabled future of ultrasound in thyroid imaging: How artificial intelligence is assisting radiologists in thyroid nodule management. Author: Timothy W. Deyer, MD, MSE Clinical Assistant Professor, Dept. of Radiology, Weill Cornell Medical Center, New York, NY Chief Medical Information Officer, Head of Interventional Radiology, East River Medical Imaging, New York, NY.
11. Koios Medical internal data. Available upon request.
Caption Guidance, Invenia, LOGIQ, and Voluson are trademarks of GE HealthCare. Koios DS is a trademark of Koios Medical. TI-RADS is a trademark of the American College of Radiology.
Product and features may not be available in all countries and regions. Full product technical specification is available upon request. Contact a GE HealthCare representative for more information.
JB28437XX