The Vital Role of Neuroimaging in the Diagnosis and Management of Acute Stroke
Stroke is a leading cause of death worldwide. According to the World Stroke Organization, more than 13 million people will have their first stroke this year and more than five million will die as a result[1]. Making a timely diagnosis is essential. All stroke patients require medical imaging to help establish whether their stroke is the result of a blockage or bleed; ischemic or hemorrhagic, respectively. Neuroimaging plays a vital role in that determination. Clinicians rely on computed tomography (CT) imaging as one of the means to help diagnose stroke type and to understand the extent and location of the damage caused by strokes, determining their severity, ranging from minimal to catastrophic.
In recent years, there have been updates to stroke clinical guidelines and advanced imaging techniques as well as interventional procedures such as endovascular therapy that are revolutionizing stroke treatment. Imaging techniques such as non-contrast CT (NCCT), CT angiography (CTA) and CT perfusion (CTP) are used to quickly evaluate patients and help clinicians determine each patient’s most promising treatment path. The use and availability of high-performance CT has improved the understanding of stroke evaluation. Stroke data demonstrates that treatment, if administered without delay, is not only possible, but also successful in a wide range of stroke patients[2]. Recent stroke trial data is also demonstrating promising results for patient treatment potential beyond the current onset guidelines[3][4].
The importance of brain imaging in TIA and stroke assessment
When patients suffer a brief episode of neurological dysfunction resulting from an interruption of blood supply to the brain, known as a transient ischemic attack (TIA), the National Clinical Guideline for Stroke (NCGS) indicates they require immediate evaluation by a specialist. That clinician will order a neuroimaging exam if they think it will alter the patient’s management. CT imaging provides clinicians with essential information to accurately triage patients and guide treatment decision-making that can improve outcomes in patients presenting with acute stroke.
When acute stroke is suspected, NCCT is commonly used to evaluate the patient’s condition and differentiate between an ischemic or hemorrhagic stroke. The NCGS recommends that the NCCT brain exam is performed immediately or at least within an hour of presentation[5]. NCCT is widely available and very sensitive in detecting hemorrhage[6]. Thin slice CT can detect large vessel occlusions (LVOs), or blockages with high sensitivity and specificity, as well as detect markers for hemorrhagic risk in patients that could undergo thrombolysis treatment[7][8].
Contrast-enhanced imaging techniques to detect vessel thrombosis in stroke
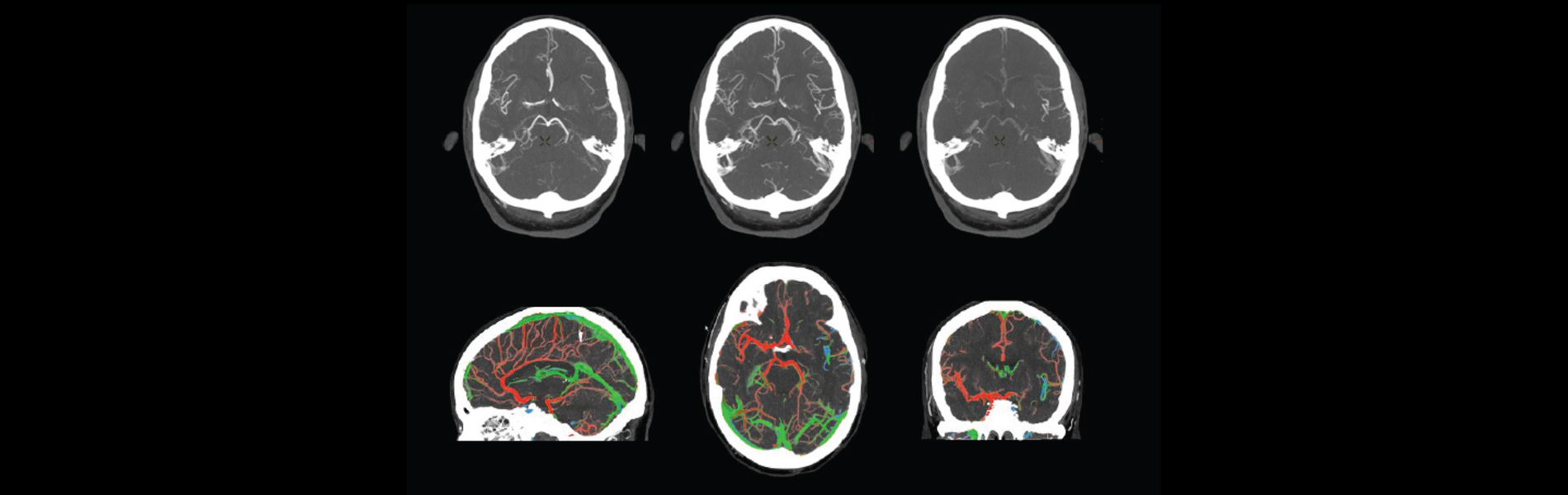
Head and neck CTA is a contrast-enhanced imaging technique that has a variety of clinical benefits. It can be performed quickly and is less expensive than other imaging techniques. It has been instrumental in aiding with stroke management and it is often used to help detect intracranial artery occlusion and large vascular occlusion. It demonstrates the location of the blockage and can help clinicians in defining the need for revascularization using endovascular thrombectomy, an image-guided procedure for blood clot removal. CTA is also integral in evaluating the extent of vessel stenosis, or narrowing, which is relevant both in the evaluation of acute stroke patients, as well as in assisting clinicians in determining their long-term prognosis. CTA can be performed in a single phase or multiphase technique, employed dependent on each patient’s stroke presentation. Single phase CTA provides information on the presence of large vessel occlusions that could be treated endovascularly, while multiphase CTA provides an assessment of brain tissue that could be potentially salvagable with intervention.
CTP is another dynamic contrast-enhanced imaging technique that provides information about the perfusion, or blood flow in the brain tissue. This technique uses sequential brain imaging to evaluate the flow of contrast through cerebral vessels, calculate the total cerebral blood volume, and calculate blood flow to a specific region. Using CTP, clinicians can estimate how much injury to brain tissue is reversible by identifying tissue with a 30 percent lower cerebral blood flow than the normal brain tissue[9].
Automation and Artificial Intelligence aid image reconstruction and communication process
In acute stroke, patient outcomes are tied to the rapid acquisition and accurate interpretation of these imaging studies. Radiologists need to not only have knowledge about the imaging techniques for acute stroke, but also the interpretation skills needed to achieve the best patient outcomes[10]. The ability to interpret sophisticated brain imaging and have an awareness of the typical findings, pearls, and pitfalls of CT image interpretation is critical for radiologists, stroke neurologists, and emergency department providers to make accurate and timely decisions regarding both (a) immediate treatment up to 4.5 hours after a stroke at primary stroke centers and (b) transfer of patients with LVO after CTA to comprehensive stroke centers for endovascular thrombectomy up to 24 hours after a stroke[11].
Innovations in imaging reconstruction have streamlined the stroke workflow to automate essential views and assist with communication between care team members. Time is critical for the evaluation and treatment of all stroke patients. New visualization tools, such as sophisticated fused views using color visualization can help clinicians assess vascular enhancement timing and enable clinicians to move patients to treatment with enhanced clinical confidence.
The progression of endovascular treatment for acute ischemic stroke
Interventional procedures such as endovascular thrombectomy have been increasingly used for the management of acute ischemic stroke due to large vessel occlusion. The increased use of this technique is in large part due to the advanced imaging techniques that have enabled the selection of patients suitable for treatment in the optimal specified window of time. Up until now, these windows of time have been very narrow and are specified in the current treatment guidelines for stroke management.
However, the most current clinical trials in stroke care are demonstrating that in place of time from stroke onset as a hard threshold to select patient’s treatment, the use of advanced imaging techniques and careful imaging-based selection can be one of the factors that is used to determine treatment eligibility in stroke care, including later windows of time from the patient’s last known state of being well. For example, in the 2019 trials referred to as the WAKE-UP and EXTEND trials, results showed that thrombolysis guided by imaging (using Magnetic Resonance Imaging and CTP respectively) is safe and effective for up to nine hours from stroke onset/last known well time [12][13]. Late window trials are demonstrating the possibility to expand patients’ treatment eligibility based on an imaging signature, such as with CT perfusion imaging[14], [15],[16]
Further research is needed to evaluate additional variables in managing stroke patients, but imaging techniques are helping clinicians in identify treatment paths as fast as possible. Image processing, especially with the use of AI and automated viewing will continue to aid in fast and reliable interpretation of stroke imaging.
To learn more about our fully automated processing platform for CT ischemic stroke studies, visit our FastStroke solution.
To learn more about GE Healthcare’s stroke solutions, click here.
To learn more about GE Healthcare’s Computed Tomography (CT) solutions, click here.
[1] https://www.world-stroke.org/world-stroke-day-campaign/why-stroke-matters/learn-about-stroke#:~:text=Globally%201%20in%204%20adults,million%20annually%20without%20appropriate%20action.
[2] Kaiser D, Gerber JC, Puetz V. Role of Neuroimaging in Guiding Treatment Decisions on Endovascular Thrombectomy. Neurology International Open 2017;1:E18–E27.
[3] Thomalla G, et al. MRI-Guided Thrombolysis for Stroke with Unknown Time of Onset. N Engl J Med 2018;379:611-22. Ma H, et al. Thrombolysis Guided by Perfusion Imaging up to 9 Hours after Onset of Stroke. N Engl J Med. 2019;380(19):1795-1803.
[4] Thomalla G, et al. MRI-Guided Thrombolysis for Stroke with Unknown Time of Onset. N Engl J Med 2018;379:611-22.
[4] Ma H, et al. Thrombolysis Guided by Perfusion Imaging up to 9 Hours after Onset of Stroke. N Engl J Med. 2019;380(19):1795-1803.
[5] White P, Nanapragasam A. What is new in stroke imaging and intervention?. Clin Med (Lond). 2018;18 (Suppl 2):s13-s16. doi:10.7861/clinmedicine.18-2-s13
[6] Yu W, Jiang WJ. A Simple Imaging Guide for Endovascular Thrombectomy in Acute Ischemic Stroke: From Time Window to Perfusion Mismatch and Beyond. Front. Neurol. 2019; 10:502. doi: 10.3389/fneur.2019.00502
[7] ACR Appropriateness Criteria® on cerebrovascular disease.
DeLaPaz RL, Wippold FJ 2nd, Cornelius RS, Amin-Hanjani S, Angtuaco EJ, Broderick DF, Brown DC, Creasy JL, Davis PC, Garvin CF, Hoh BL, McConnell CT Jr, Mechtler LL, Seidenwurm DJ, Smirniotopoulos JG, Tobben PJ, Waxman AD, Zipfel GJ
J Am Coll Radiol. 2011 Aug; 8(8):532-8.
[8] von Kummer R, Bourquain H, Bastianello S, et al. . Early prediction of irreversible brain damage after ischemic stroke at CT. Radiology 2001;219:95–100 [PubMed]
[9] Bivard A, Levi C, Spratt N, Parsons M. Perfusion CT in acute stroke: a comprehensive analysis of infarct and penumbra. Radiology. 2013 May;267(2):543-50. doi: 10.1148/radiol.12120971. Epub 2012 Dec 21. PMID: 23264345.
[10] Na DG, Sohn CH, Kim EY. Imaging-based management of acute ischemic stroke patients: current neuroradiological perspectives. Korean J Radiol. 2015;16(2):372-390. doi:10.3348/kjr.2015.16.2.372
[11] https://pubs.rsna.org/doi/full/10.1148/rg.2019190142
[12] Thomalla G, et al. MRI-Guided Thrombolysis for Stroke with Unknown Time of Onset. N Engl J Med 2018;379:611-22.
[13] Ma H, et al. Thrombolysis Guided by Perfusion Imaging up to 9 Hours after Onset of Stroke. N Engl J Med. 2019;380(19):1795-1803.
[14] Thomalla G, et al. MRI-Guided Thrombolysis for Stroke with Unknown Time of Onset. N Engl J Med 2018;379:611-22.
[15] Albers GW, et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N Engl J Med 2018;378:708-18.
[16] Nogeira RG, et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N Engl J Med 2018;378:11-21.